Hypertension (more commonly referred to as high blood pressure) affects approximately half of all adults in the U.S. today, with many of those same individuals carrying an increased risk of developing heart disease or suffering from a stroke. These two adverse effects linked to hypertension are the leading causes of death in the U.S. and in 2023, nearly 665,000 deaths considered high blood pressure as the primary or contributing cause.1 High blood pressure is often considered a "silent killer" given that physical symptoms may not be present or recognizable.
Help Your Members Take Control of Their Blood Pressure
Through just one compliant systolic/diastolic reading during the measurement year, closing the CBP measure remains an in-year program opportunity for health plans still looking to meet their quality improvement goals. However, when hard-to-reach members or those who live in rural areas skip in-office visits with their PCPs, health plans risk missing the mark on hitting their compliance targets.
Controlling high blood pressure is one of the most important steps health plan members can take to reduce their risk of long-term health complications including heart attacks, stroke, and kidney disease. Health plans can help their members manage their hypertensive diagnoses through prescribed medication adherence while encouraging low-sodium diets, increased physical activity, and participation in smoking cessation programs where applicable.2
Get a Better Reading on CBP Measure Compliance
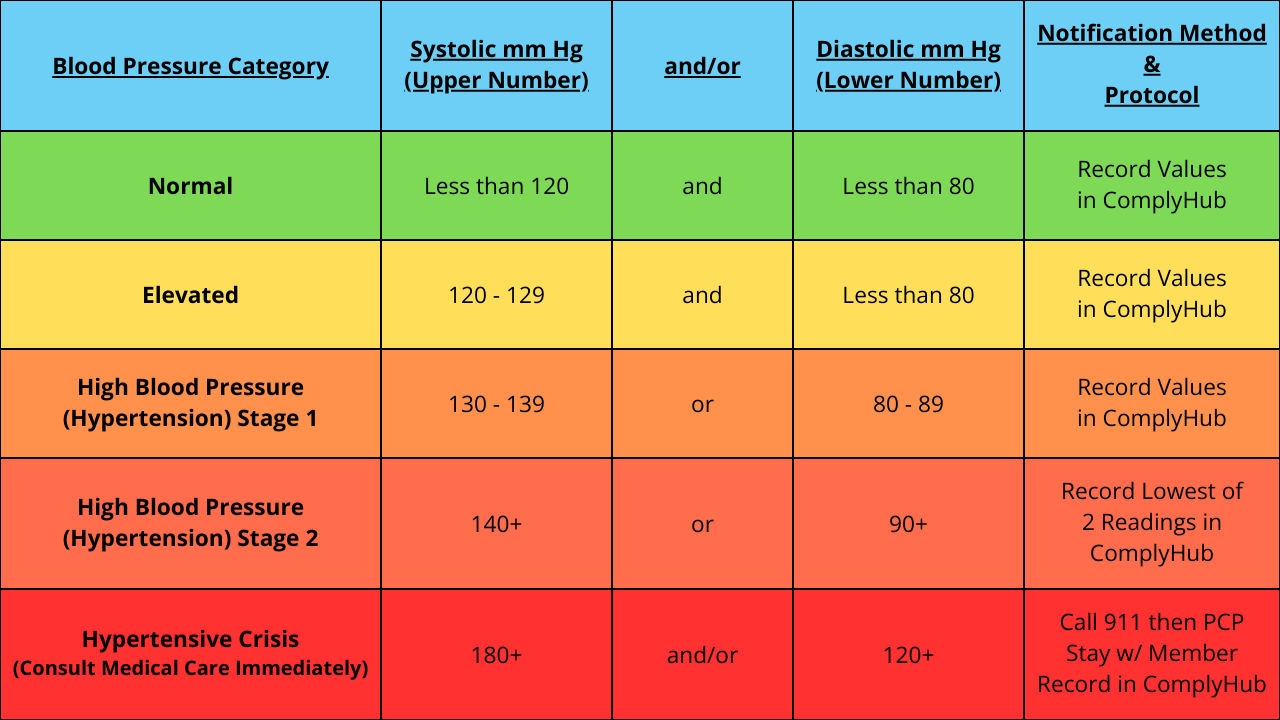
In order to meet NCQA's HEDIS measure requirements for CBP, eligible members aged 18-85 that are diagnosed with hypertension must have a blood pressure reading of <140/90 mm Hg documented during the measurement year. These readings must be taken by a healthcare professional using appropriate equipment and protocols, given that self-reported or home-monitoring results are not considered compliant unless performed by a clinician during an in-person visit.
To successfully close the CBP care gap, health plans must identify the most recent blood pressure reading noted in 2025. If multiple blood pressure readings have been recorded on the same date of service, health plans should use both the lowest systolic and diastolic values available. Blood pressure readings taken from remote monitoring devices and electronically submitted directly to the member's provider may be used. However, these submissions must clearly document that the reading was taken using an electronic device and subsequently interpreted by a provider.3
For HEDIS MY 2025, NCQA has proposed a new Electronic Clinical Data System (ECDS) reported measure titled Blood Pressure Control for Patients with Hypertension (BPC-E). This proposed measure is an improvement on the existing Controlling High Blood Pressure (CBP) HEDIS measure, which uses the hybrid reporting method (including medical record review) with three key modifications:
- The measure uses the ECDS reporting method.
- The denominator includes a pharmacy data method.
- The numerator includes two rates:
- Blood Pressure <140/90 mm Hg
- Blood Pressure <130/80 mm Hg
NCQA's long-term goal is to include only the new proposed measure in HEDIS, as the existing CBP measure will remain in place while they develop a transition plan.4

In-Home Blood Pressure Monitoring: Full At-Risk
Retina Labs in-home blood pressure monitoring program helps health plans connect with their hypertensive member populations using proven multi-channel member engagement strategies, ensuring that our preventive screening services effectively close the CBP care gap.
With a focus on member convenience, our highly trained Field Technologists follow American Heart Association (AHA) protocols to ensure accuracy and consistency while also meeting CMS & NCQA standards for quality compliance. They are equipped to recognize and act on hypertensive emergencies during an in-home member visit, in which case our Field Technologists will adhere to established care coordination and escalation procedures.
Using real-time program performance tracking through our ComplyHub platform, our solution aligns with your quality team's population health needs to better understand both individual and aggregate member-level data. This is met through detailed documentation captured by our Field Technologists during each in-home visit with your members including readings, pulse, and cuff size - all of which can be sent directly to each member's PCP using secure DirectTrust messaging protocols.
Best of all, Retina Labs delivers our in-home blood pressure monitoring services fully at-risk through a pay-for-performance gap closure program model. This comprehensive approach complements our existing in-home preventive screening services including diabetic eye exams and bone density scans, ensuring that multiple gaps in care are closed in a single visit while prioritizing access to care.
Need a Pulse on Your CBP Star Ratings?
Retina Labs is here to help! Contact us today to learn more about our convenient member-centric approach to in-home preventive screenings designed to close the CBP care gap more efficiently while boosting your Star Ratings.
References:
- High Blood Pressure Facts | CDC
- Controlling High Blood Pressure (CBP) | NCQA
- Controlling High Blood Pressure (CBP) 2025 PDF | Anthem
- Proposed New Measure for HEDIS MY 2025 (BPC-E) | NCQA.pdf
Infographic/Table References:
.png)
.png)
.png)
.png)
%20(1).png)
.png)
.png)
.png)
.png)
.png)






















.png)
.png)





.jpg)
.png)
